When Reviewing Medical Records or Verifying the Diagnoses the Evaluators Should Be Blin
Skip to Highlights
What GAO Found
The Centers for Medicare & Medicaid Services (CMS) is collecting Medicare Reward (MA) run across information—data on the services and items furnished to enrollees—that are more comprehensive than the casher diagnosis information the agency currently uses to gamble adapt capitated payments to MA organizations (MAO). CMS, an agency within the Section of Health and Human Services (HHS), makes these adjustments to reverberate the expected health care costs of MA enrollees. Encounter information have many more than elements—including procedure codes and provider payments—from a wider range of provider types—such equally home wellness agencies and skilled nursing facilities—thus expanding the scope of sources for diagnosis and other information.
CMS has not fully developed plans for using MA run into data. The agency announced that it will begin using diagnoses from both encounter information and the data it currently collects for take a chance adjustment to determine payments to MAOs in 2015. However, CMS has non established fourth dimension frames or specific plans to employ encounter information for other potential purposes.
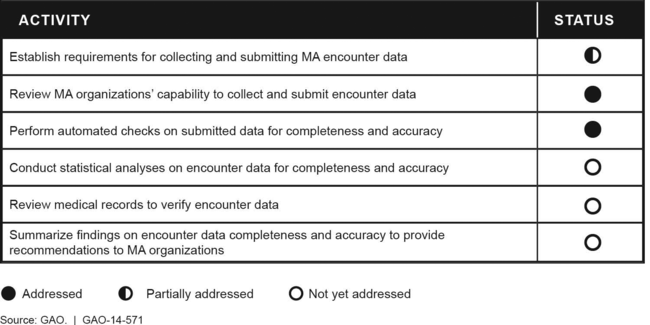
CMS has taken some, but not all the same all, advisable deportment to ensure that MA encounter data are complete and accurate. (See figure.) The agency has established timeliness and frequency requirements for data submission, but has not yet developed requirements for completeness and accurateness. Also, the agency has certified nearly all MAOs to transmit encounter data. Although CMS performs automated checks to make up one's mind whether key data elements are completed and values are reasonable, information technology has not even so performed statistical analyses that could detect more than complex data validity issues. For case, CMS has not however generated basic statistics from the data by demographic grouping or provider type to identify inconsistencies or gaps in the data. Also, it has non yet reviewed medical records to verify diagnoses and services listed in encounter information or reported what it has learned near data quality to MAOs. Agency officials told GAO they intend to perform these boosted quality assurance activities merely have not established time frames to practice so.
Status of the Centers for Medicare & Medicaid Services' Activities to Validate Medicare Reward (MA) Encounter Information, May 2014
Why GAO Did This Written report
Medicare Reward—the private plan culling to the traditional Medicare programme—provides health care for virtually 15.five meg enrollees, about 30 percent of all Medicare beneficiaries. Afterwards a multiyear rollout, CMS began collecting encounter information in Jan 2012. GAO was asked to review CMS'southward plans for using MA come across information and its efforts to validate the data's quality.
This report examines (one) how the scope of MA see data compare with CMS's current risk adjustment information, (2) the extent to which CMS has specified plans and time frames to apply see data for adventure adjustment and other purposes, and (3) the extent to which CMS has taken appropriate steps to ensure MA come across information'southward completeness and accurateness. In addition to reviewing laws, regulations, and guidance on MA run into data collection and reporting, GAO interviewed CMS officials and representatives of MAOs. GAO also compared CMS's activities to the protocol CMS adult to validate Medicaid encounter data—comparable information nerveless and submitted by entities like to MAOs.
Skip to Recommendations
Recommendations
CMS should establish specific plans for using MA meet data and thoroughly assess data completeness and accuracy before using the data to risk suit payments or for other purposes. While in general agreement, HHS did not specify a appointment by which CMS will develop plans for all authorized uses of encounter data and did non commit to completing data validation earlier using the information for risk adjustment in 2015.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare and Medicaid Services | Priority Rec. | HHS generally agreed with this recommendation. Every bit of Feb 2022 CMS has finalized its timeframe for using MA encounter information for risk adjustment. CMS is also using MA meet data for purposes other than risk adjustment, such as quality measurement and program integrity, and continues to develop boosted uses, but has not established specific plans and time frames for all uses. Quality measurement - CMS uses MA meet data to obtain diagnoses for Part D Medicaid Adherence measures and reports using meet data for other Part D measures. CMS has also used MA encounter data as office of evaluating the first three years of MA's Value-Based Insurance Blueprint Model-wellness insurers' efforts to structure health programme elements to encourage enrollees with chronic conditions to use peculiarly beneficial services. Public health - CMS uses MA encounter data to assist identify beneficiaries at risk in areas affected by public health emergencies and disasters. CMS also plans to has use MA encounter data for other public wellness purposes, such as identifying beneficiaries with a history of opioid-related overdose, thereby identifying them every bit potentially at-adventure for prescription drug abuse. CMS reports that its Office of the Actuary (OACT) has used MA encounter information to study the impact of emergencies including hurricanes and COVID-nineteen on utilization of services to inform projections of Medicare expenditures. Program management - CMS reports that OACT incorporates MA meet information into multiple core responsibilities, including evaluation of MA bids, analysis of Medicare trends, comparison of FFS and MA experience, and the evolution of rates for demonstration programs. Program Integrity - CMS has begun using MA encounter information for plan integrity purposes. For example, a program integrity contractor (MEDIC) utilizes MA encounter data to identify providers with patterns of encounters that may exist indicative of fraud, waste, and abuse; conduct information assay to develop investigations; and identify MA providers who also submit Medicare Parts A and B claims where administrative actions or law enforcement referrals take occurred. As some other example, CMS reports using MA run into data in Fraud Prevention Organization opioid-related models as an exclusion in identifying providers. Additionally, CMS states that the Part D quarterly reports include opioid-related analyses which employ come across information as an exclusion. Despite connected progress in using MA meet data, plans for comprehensive oversight purposes remain express. For example, CMS has not established specific plans for using MA encounter data to monitor Medicare coverage or support more comprehensive plan integrity efforts. Nosotros will continue to monitor CMS's progress in developing specific plans and fourth dimension frames with dates for all intended purposes of MA encounter data. |
| Centers for Medicare and Medicaid Services | Priority Rec. | HHS generally agreed with this recommendation, however, HHS did not commit to completing information validation before using MA come across information for chance aligning. Every bit of February 2022, CMS has made additional progress in examining the completeness and accuracy of Medicare Advantage encounter information, only more work remains to fully validate these data. CMS has developed and is implementing a Medicare Advantage Encounter Information Integrity and Monitoring plan, which describes the primal activities of evaluating and improving come across data, including outreach, data analysis, and monitoring completeness and accurateness. As part of this plan, CMS has established preliminary performance metrics for MA encounter data completeness and accuracy and is conducting associated analyses. Further, the bureau has communicated findings from these analyses to MAOs, with the expectation that MAOs provide plans inside 60 days to address identified concerns. CMS has non verified MA see information by reviewing medical records, however, the agency plans to brainstorm verifying payment year 2016 data through Risk Adjustment Information Validation audits by Fall 2021. While these steps are important, without fully validating the completeness and accuracy of MA encounter data, CMS would exist unable to confidently employ these data for risk aligning or other plan management or policy purposes. We will continue to monitor CMS's progress in fully validating MA encounter information. |
Total Written report
Source: https://www.gao.gov/products/gao-14-571
0 Response to "When Reviewing Medical Records or Verifying the Diagnoses the Evaluators Should Be Blin"
Postar um comentário